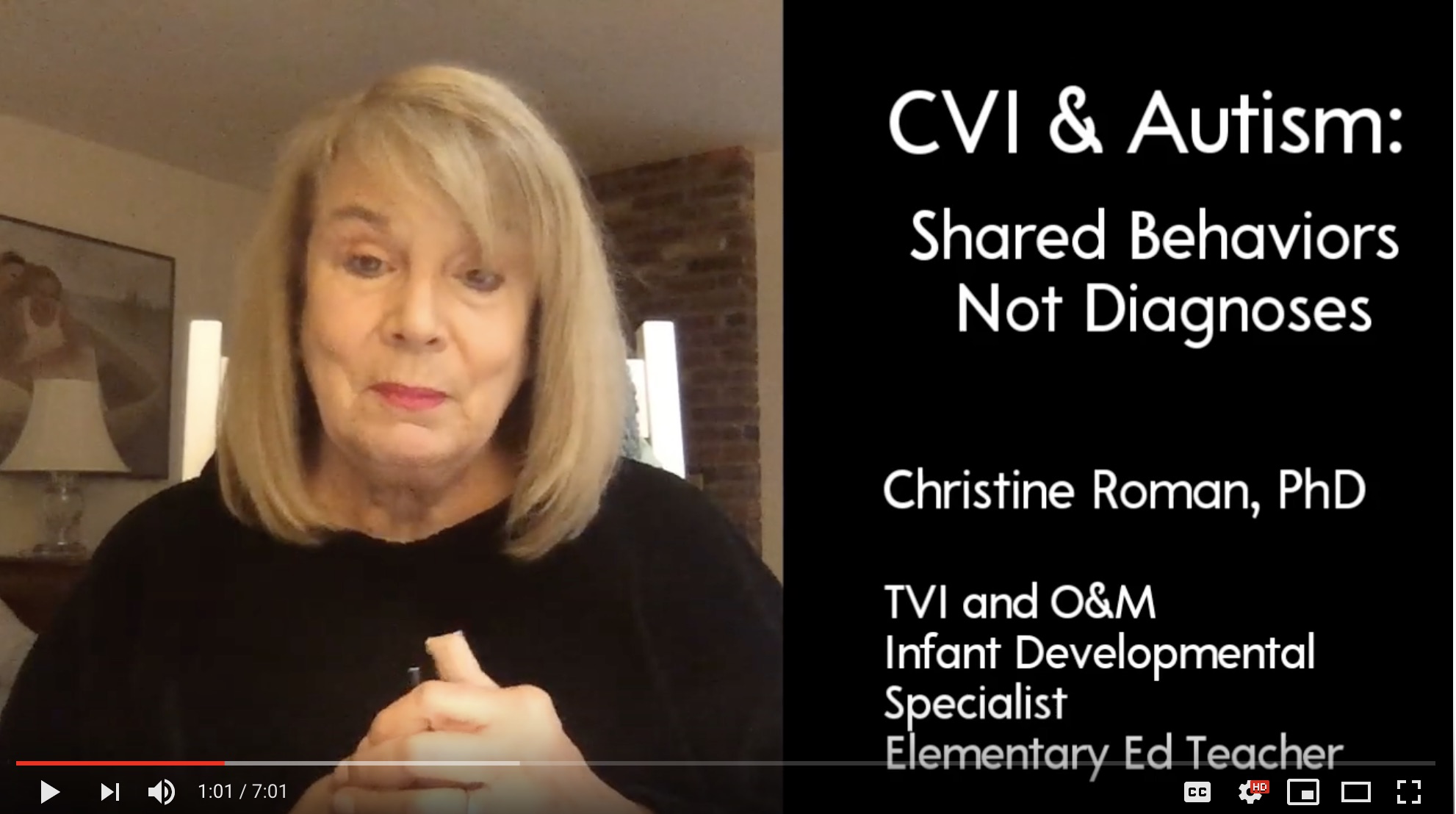
CVI and Autism: Shared Behaviors, Not Diagnoses
Dr. Christine Roman discusses the shared behaviors in cortical visual impairment (CVI) and autism in this YouTube video.
Dr. Christine Roman discusses the shared behaviors in cortical visual impairment (CVI) and autism in this YouTube video. This is Episode 13 in the “Roman on CVI” video series.
Transcript
Welcome to Roman on CVI. Today I’d like to talk a little bit about two diagnoses that are often brought together. Those are cortical visual impairment and autism. Why do they seem to get conflated? Why do they seem to come together in the same child maybe more often than is even appropriate?
I’d like to suggest that shared behaviors are not the same as shared diagnosis and yet we do see that frequently. Let me see if I can maybe unwind some of the problem here. What is the inherent difficulty? Why does this happen? Why do some diagnosticians think that they’re seeing autism, when others might believe they’re seeing CVI and very often not both together? Really just one. So what are some of these shared behaviors?
Shared Behaviors Between CVI and Autism
Well, let’s think about this. If you were a diagnostician and you saw a child who didn’t follow a point; they didn’t see someone watching where someone else is pointing; if they had trouble with eye-to-eye contact; if they had play behaviors that were unusual — a lack of representational or pretend play, possibly repetitive play or play that seems to not vary too much; if that person likes to go to the same place all the time; they resist going to new places; if they like things that move; if they have delays in communication — both expressive and receptive communication– some people might think, “Oh, I know what that is. That’s autism.” But those of you who are watching this video, who know CVI, also know that I was describing the characteristics of CVI.
Sorting Out the Difference Between CVI and Autism
So how do we sort that out? Well, I think it’s critical that the person who is doing the diagnostic testing has knowledge, not only in the area of CVI, but in the area of autism, or the reverse: if their expertise is first autism, they should also know about CVI, due to the concern that these things might artificially come together. One of the things that might help is that children with CVI have conditions that are pretty well identified that are causes of CVI and those include, you know, interventricular hemorrhage, genetic disorders, hydrocephalus, asphyxia. We know that collection of medical things that place a child at risk for CVI. We don’t know what the causes of autism are yet. There’s, you know, work really aggressively being conducted to help understand that. So my suggestion to diagnosticians is when you see one of those medical conditions, you know, white matter damage or intraventricular hemorrhage or the other ones that we mentioned is well — stroke — that the diagnostician first think, “Oh, red flag for CVI. I wonder if I should have somebody here with me who knows CVI or make sure that this person has a CVI range if I have any doubts at all about what I’m seeing.” The key is to make sure that diagnostician pauses and thinks about which one of these things that medical cause is leading to.
Different Interventions for CVI and Autism
I also want to mention that, you know, this matters in many ways, not just because we want to get it right, but, you know, why does it ultimately matter? It ultimately matters because the interventions for each group are quite different. People with CVI have a barrier to access. They can’t access the visual information in their world incidentally and so often they can only access it when the conditions are appropriately met, and those conditions, such as using vibrant color, movement, by using low complexity, by reducing the sensory environment, don’t just help that child feel more centered, like they would for a person with autism perhaps, but they actually create access and that’s the key is that children with CVI need a program that provides visual access to learning. Without that, any autism interventions result in a change of behavior, but not necessarily improvements in learning, so I’d like to just, you know, suggest that we all think very hard about the children that we have on our caseloads or that you meet who are diagnosed with these dual diagnoses of CVI and autism. Could they actually come together in the same child? Sure, they could, but probably not with the frequency that we’re seeing and look, I suggest you also look at some other behaviors. So I suggest if you look at attachment behaviors, for example, does this child with CVI who’s maybe being thought to have autism, do they have attachment issues? Do they treat family members the same way they would treat a stranger, like some kids with autism do? Or is attachment not an issue? Are there social..is there social engagement? You know, is a child interested and notices social engagement and doesn’t you know cover their ears as though it is too much sensory information? Kids with CVI might cover their ears, but it’s often because the visual world is compounded with the auditory world that’s making them unable to see.
CVI Is a Barrier to Access
One is access. One is really about helping to center and control that child’s ability to modify – to integrate — sensory information. They’re really different things. Easy to see why people would make a mistake — very easy to see, but finally I would suggest that if you have a student on your caseload or your child has been diagnosed with autism and is not making progress, is not learning, at the rate at which people would expect them to learn, maybe take a second look at that autism diagnosis, if the other criteria are met, if the child has an eye exam that doesn’t explain the way the child uses our vision functionally, has a history of a neurologic condition associated with CVI, maybe they also have the ten visual and behavioral characteristics, in which case their program can be adjusted and hopefully progress will occur.
Thank you.
