What is Central Auditory Processing Disorder and Why Is It Important?
What is Central Auditory Processing Disorder and Why Is It Important?
It is said that central auditory processing disorder is to hearing what cerebral visual impairment or CVI is to vision. Central auditory processing disorder (CAPD) is defined as deficits in the neural processing of auditory information in the central auditory nervous system (ASHA, 2019). Central auditory processing disorder is also called auditory processing disorder (APD), cortical deafness, and central deafness. In these definitions, “central” refers to the site of the problem with hearing and comprehension. While the peripheral hearing system includes the outer, middle, and inner ear to the auditory nerve, the central hearing system refers to the area from the brainstem to the brain. With CAPD, the ears may be functioning normally but sound is not reaching the brain in a way that is meaningful.
Students who are blind or visually impaired—and who have typically developed hearing—depend in part on their hearing to compensate for what they miss visually. For students who also experience varying degrees of CAPD, compensating with auditory information, whether speech or environmental cues, may not be possible. Unfortunately, CAPD cannot be diagnosed in very young children and CAPD assessments in older children require language acquisition, which many of these children haven’t yet acquired. What do we do with children who are at significant risk for CAPD but who cannot be accurately tested for a definitive diagnosis? There are evidence-based auditory strategies that can be used with children who are suspected of having CAPD that are similar to the visual strategies used with children with CVI.
It is also important to distinguish between CAPD and auditory neuropathy spectrum disorder because these two conditions are often confused but are very different. In CAPD, the hearing problem is brain-based, with the peripheral hearing system intact. With auditory neuropathy, there is damage to the inner hair cells of the cochlea and also possible damage to the auditory nerve. Unlike CAPD, auditory neuropathy can be diagnosed in young children who may not yet be efficient communicators. Tests that measure auditory brainstem responses (called ABRs) and reflexes of the muscles of the middle ear (often called acoustic reflex testing) will be normal in CAPD but abnormal or absent in auditory neuropathy (Morelt, 2010). These tests allow audiologists to make a reliable differential diagnosis between auditory neuropathy and possible CAPD in children who may seem to have features of both CAPD and auditory neuropathy.
Risk Factors Associated with Both Central Auditory Processing Disorder and CVI
Many of the risk factors for CVI and CAPD are the same (American Speech-Language Hearing Association, 2019; Boston Children’s Hospital, 2019; Jin et al., 2019; Khetpal & Donahue, 2007) and therefore children with significant multiple disabilities who are diagnosed with CVI may also be at risk for CAPD.
The following risk factors are associated with both CVI and CAPD:
- Hypoxia (i.e., not enough oxygen reaching the tissues of the body) • Anoxia (i.e., an absence of oxygen, an extreme form of hypoxia) • Prematurity
- Seizure disorders
- Prenatal drug exposure
- Cytomegalovirus (CMV)
- Meningitis (i.e., inflammation of the membranes surrounding the brain and spinal cord)
- Low birth weight
- Traumatic brain injury
- Hydrocephalus (i.e., fluid accumulation in the brain)
- Hypoxic ischemic encephalopathy (i.e., brain damage caused by oxygen deprivation)
- Hyperbilirubinemia (i.e., the cause of jaundice)
Signs that a Child or Student Might have Central Auditory Processing Disorder
The National Institute on Deafness and Other Communication Disorders (2010) states that children with central auditory processing disorder often:
- have trouble paying attention to and remembering information presented orally, and may cope better with visually acquired information.
- have problems carrying out multi-step directions given orally; need to hear only one direction at a time.
- have poor listening skills.
- need more time to process information.
- have low academic performance.
- have behavior problems.
- have language difficulties (e.g., they confuse syllable sequences and have problems developing vocabulary and understanding language).
- have difficulty with reading, comprehension, spelling, and vocabulary.
Other features of CAPD include distractibility, difficulty localizing sounds, difficulty hearing in noisy environments with a lot of competing sounds, and difficulty understanding speech that is too fast (ASHA, 2019).
Strategies to Support Students with Suspected Central Auditory Processing Disorder
Teachers of the visually impaired routinely provide VI services for children with CVI, which is one of the leading causes of visual impairment in children in the U.S. Teachers of the Deaf/hard of hearing, however, are much less likely to serve children who are diagnosed with CAPD as the sole cause of their hearing loss. While speech and language therapists may be available to support these students if speech and language services are included in the related services of these students’ IEPs, there are strategies that can be implemented by all team members.
While the following strategies are designed to support students with CAPD, they will likely benefit most blind and visually impaired students in educational programs. These strategies help ensure that all students have access—to the maximum extent possible—to auditory information.
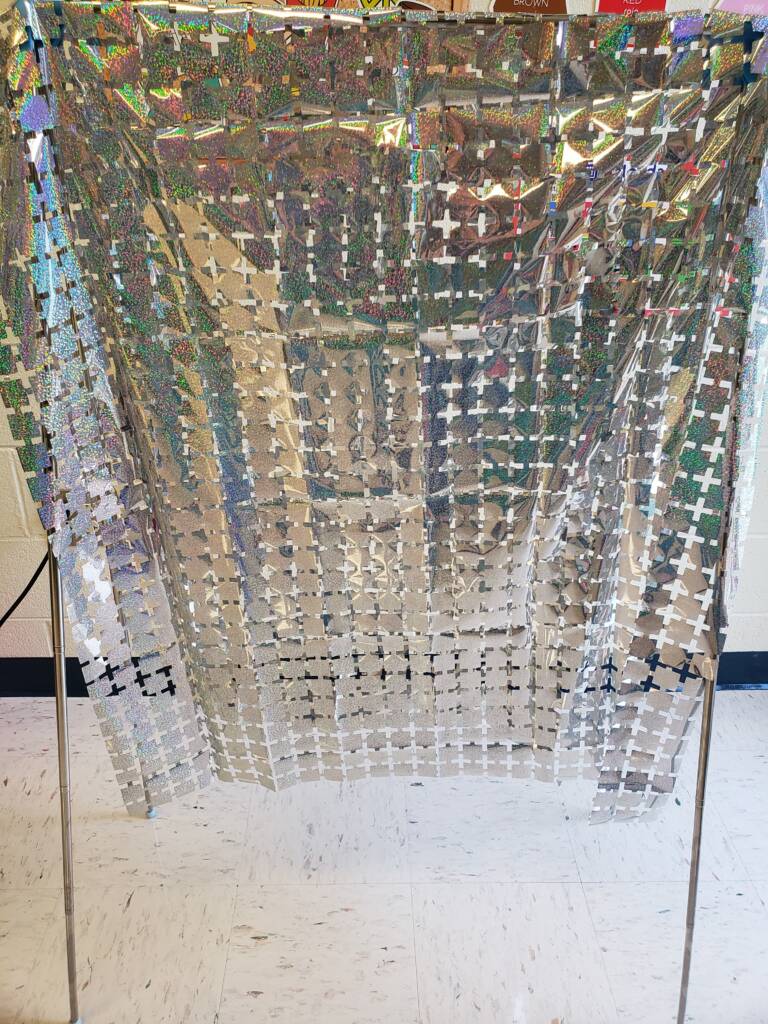
- Decrease auditory clutter. Auditory clutter can impact a student’s ability to process spoken language and environmental sounds in the same way that visual clutter can make it difficult for a child with CVI to use their vision to the maximum extent possible. Amplification technologies, such as soundfield systems, can raise (i.e., improve) the signal-to-noise ratio so that the student can hear what’s most important over less important competing noise. There are also a number of strategies for reducing classroom noise, such as rubber tips or tennis balls on the legs of chairs, establishing set times for noisy activities like pencil sharpening, and covering shelves with homemade drapes to improve acoustics.
- Allow sufficient time for auditory processing. Give students adequate time to process information and respond. Consider each student’s auditory processing and their need for “wait time”. Fifteen to 30 seconds of wait time, which is not at all unusual among this population of students, can seem much longer when waiting for a student to respond to a request or command.
- Consider your rate of speech. The central nervous system of a young child cannot process the acoustic and language elements of spoken language at a rate faster than about 124 words-per-minute (Hull, 2009; Hull, 2012). To imagine what 124 words-per-minute sound like, think of Mr. Rogers, who was a master at speaking at precisely this rate. Of course, we all talk faster than this most of the time. But consider slowing down your words-per-minute rate when presenting new or particularly important information to help support comprehension. Even older students of high school age only process language at a rate maximum rate of about 145 words-per-minute. And remember that we’re only talking about slowing down the rate of speech, not slowing down the pronunciation of individual words. We still speak clearly without artificially over-enunciating words and syllables.
- Consider the limits of simultaneous multi-sensory input. There may be times when it is not advisable to require multi-sensory participation. If a student with CAPD is listening very carefully, at that moment they may not be as available for visual and tactile input as they might otherwise be. This is similar to the way that children with CVI can sometimes seem more visually impaired when they are listening carefully or exploring tactile objects, especially objects that are new to them.
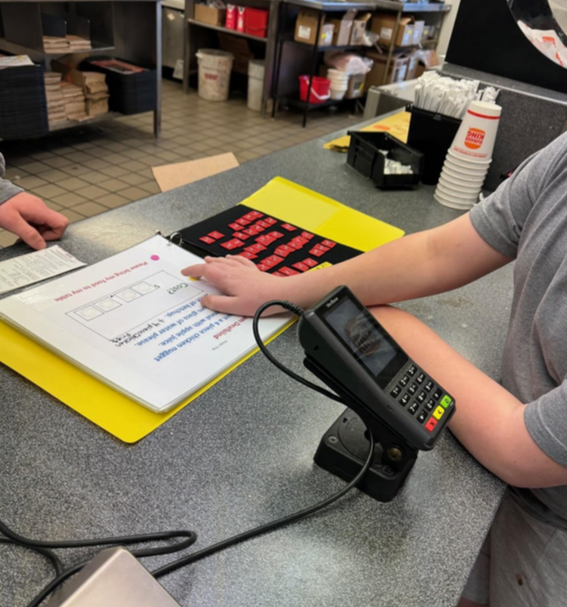
- Use a multisensory approach. Even though a student may not be able to access auditory, visual, and tactile information simultaneously, a multisensory approach is still important. In some cases, you may want to provide sensory input through one sense at a time. For example, when presenting a novel item, you may want to wait for the student to tactually explore the object before providing auditory information about what the object is called, its purpose or use, etc.
Assessment Tools for CAPD
- Auditory Processing Difficulties Checklist (PDF)
- CAPD Checklist (Word document)
For More Information
If you have a student who is diagnosed with CVI and who you think might also experience auditory processing issues, I am happy to offer guidance. I can be reached at mbelote@sfsu.edu or 415-405-7558. And the American Speech-Language-Hearing Association (ASHA) has a very informative website specific to CAPD.
References
American Speech-Language-Hearing Association. (2019). Central auditory processing disorder.
Boston Children’s Hospital. (2019). Cortical visual impairment symptoms and causes.
Dennison, E., & Hall Lueck, A. (2006). Proceedings of the summit on cerebral/cortical visual impairment: Educational, family, and medical perspectives. New York: American Foundation for the Blind Press.
Ferre, J.M. (2007). Understanding intervention for (C)APD: Easy as A-B-C. The ASHA Leader, 12(10), 20-22.
Hull, R. (2009). A child’s CNS auditory system: Do we expect too much? Paper presented at the U.S. Office of Special Education Programs, Project Directors’ Conference, Washington, DC.
Hull, R. (2012). Misdiagnosed developmental delays in young children. Paper presented at the U.S. Office of Special Education Programs, Project Directors’ Conference, Washington, DC.
Jin, H.D., Demmler-Harrison, G.J., Miller, J., Edmond, J.C., Coats, D.K., Paysse, E.A., Bhatt, A.R., Yen, K.G., Klingen, J.T., Steinkuller, P., & Congenital CMV Longitudinal Group. (2019). Cortical visual impairment in congenital cytomegalovirus infection. Journal of Pediatric Ophthalmology and Strabismus, 56(3),194-202. Retrieved from: https://www.ncbi.nlm.nih.gov/pubmed/31116869
Khetpal, V., & Donahue, S.P. (2007). Cortical visual impairment: etiology, associated findings, and prognosis in a tertiary care setting. Journal of the American Association for Pediatric Ophthalmology and Strabismus, 11(3), 235-239. Retrieved from: https://www.ncbi.nlm.nih.gov/pubmed/17459745
Lueck, A.H., & Dutton, G.N. (Eds.). (2015). Vision and the brain: Understanding cerebral visual impairment in children. New York: American Foundation for the Blind Press.
Morelt, T. (2010). Auditory Neuropathy Spectrum Disorder and (Central) Auditory Processing Disorder. Deaf-Blind Perspectives, 17(2), 1-5.
National Institute on Deafness and Other Communication Disorders. (2004). Auditory processing disorder in children.
Roman-Lantzy, C. (2007). Cortical visual impairment: An approach to assessment and intervention. New York: American Foundation for the Blind Press.